A Technical Perspective
A Technical Perspective on Nocturnal Bracing for Adolescent Idiopathic Scoliosis

Historically, full-time bracing has been the cornerstone of conservative management for adolescent idiopathic scoliosis (AIS). Numerous orthotic designs have been developed, each purporting to improve upon its predecessors. Despite the abundance of comparative studies among these full-time devices, there is limited high-quality evidence supporting the consistent superiority of one design over another. Ultimately, brace efficacy hinges on several foundational principles: achieving in-brace correction (including reductions in Cobb angle and axial rotation), maintaining sagittal and coronal balance, and ensuring sustained patient compliance.
These criteria, while conceptually straightforward, often prove difficult to implement in practice, particularly given the biomechanical and behavioral demands placed on patients required to wear a brace 18 to 22 hours daily. A major complicating factor is the need for upright posture and mobility, which introduces substantial design constraints and increases the likelihood of patient discomfort.
Creating, fitting, and adjusting to optimize the effectiveness of the brace requires a substantial level of expertise and understanding of proper force vectors and reliefs.
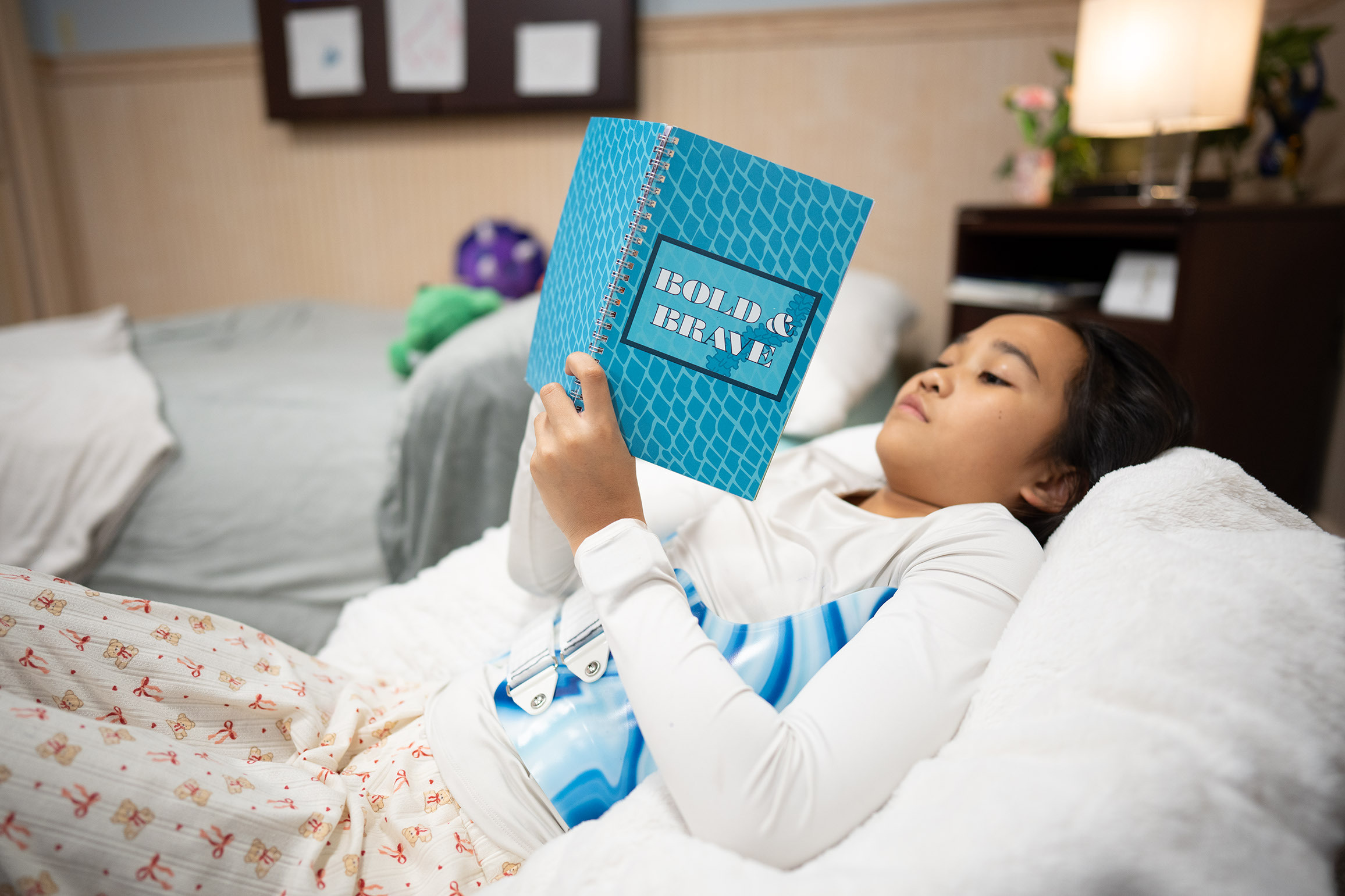
However, by far, the most challenging complication with bracing by any means is that of patient compliance. This is most apparent with full-time bracing, when a patient is required to wear the brace outside of the home and throughout the day, including to school and social events. The psychosocial impact on teens and the challenges they face are well documented and continue to be reported on.
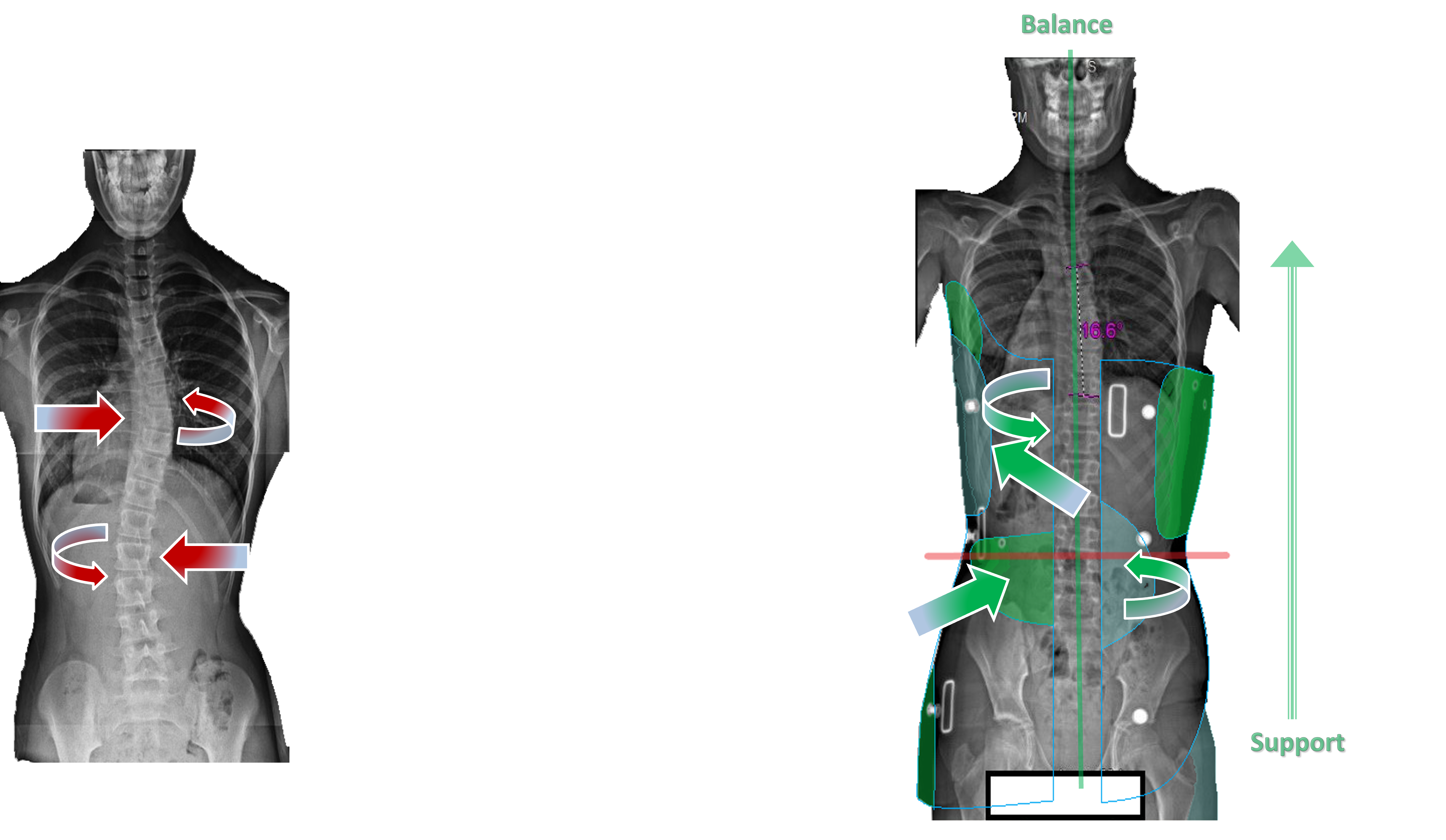
Nocturnal bracing presents a biomechanically favorable alternative that mitigates many of these limitations. When patients are recumbent, gravitational load is neutralized, allowing the spine to elongate and intervertebral discs to decompress. This position facilitates enhanced access to the lumbar spine, horizontal orientation of the ribs for thoracic manipulation, and decreased resistance from paraspinal musculature.
In this relaxed state, righting reflexes are suppressed, and considerations of stance and balance are eliminated. As a result, corrective forces can be applied with greater precision and intensity, often through simplified brace architecture.
The biomechanical rationale for this approach is underpinned by the Hueter-Volkmann principle, which describes the inverse relationship between mechanical loading and physeal growth. Asymmetric loading, characterized by compressive forces on the concave side and tensile forces on the convex side of the curve, alters vertebral growth trajectories, promoting progression in skeletally immature patients.
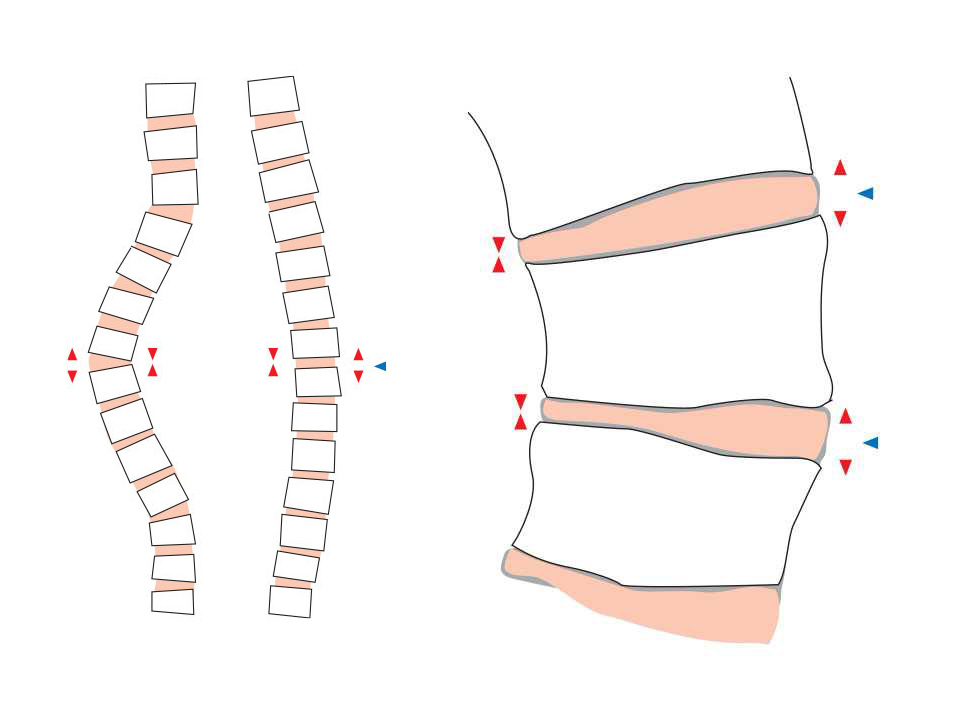
This imbalance can reach growth rate discrepancies of 40% or more. By reversing these forces through strategic unloading and hyper-correction, nocturnal bracing may not only arrest curve progression but actively promote regression. This same mechanistic model is employed in surgical interventions such as anterior vertebral body tethering (AVBT), where convex-side compression modulates growth to correct deformity.
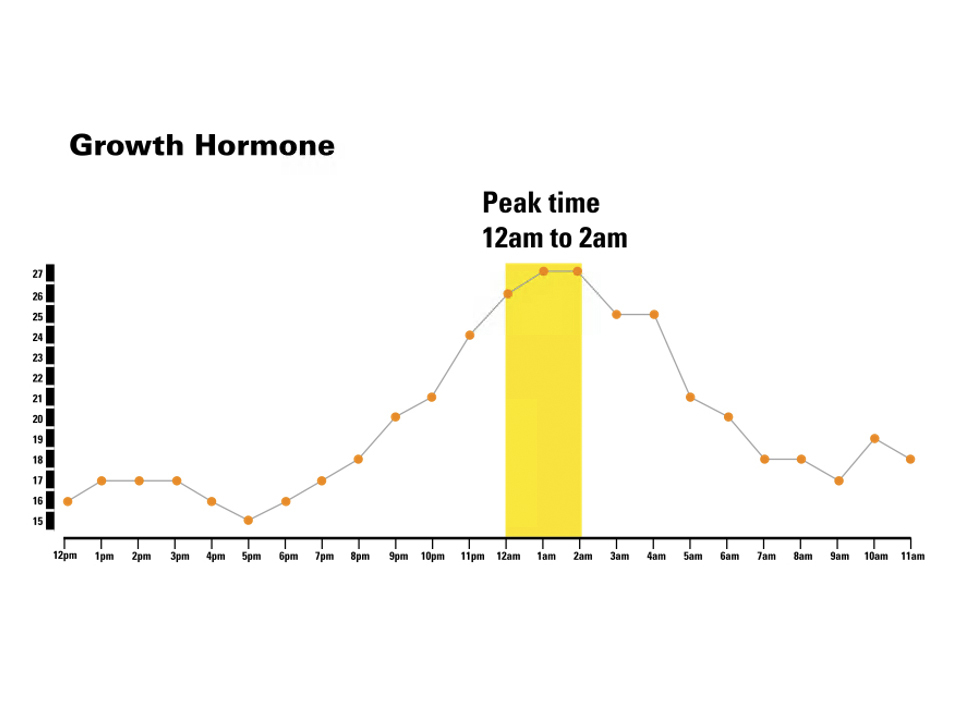
Additionally, nocturnal bracing capitalizes on circadian patterns of growth physiology. The majority of endogenous human growth hormone (GH) secretion occurs during stage 3 non-REM sleep, typically peaking between midnight and 2 a.m. This temporal alignment enhances the potential for modulating vertebral growth during bracing. For instance, devices such as the Providence Brace have demonstrated high in-brace correction rates, averaging 98%, with some cases exceeding 115%, due to the application of targeted hyper-corrective forces that would be intolerable under ambulatory conditions.
Furthermore, by restricting brace wear to the nocturnal period, patient compliance significantly improves, circumventing the psychological and physical burdens associated with daytime bracing in social and academic settings.
In summary, nocturnal bracing leverages optimal biomechanical conditions, growth physiology, and improved patient adherence to offer a compelling modality for the conservative treatment of AIS. When properly implemented, it can yield outcomes comparable to, or possibly in some cases, superior to traditional full-time bracing.